
What good is a treatment if your patient won’t adhere to it?
Some patients may perceive compression therapy or offloading as a MAJOR INCONVENIENCE, as it involves engaging with treatment for a LONG PERIOD OF TIME.1
Low adherence with therapy may results in DELAYED HEALING and poor healing outcomes2.
Healthcare professionnals have an IMPORTANT ROLE to play in explaining :
- The aetiology,
- Why the treatment is important
- Why they should wear compression or offloading continuously
- Etc
The objective is to enable them to play an ACTIVE ROLE IN THEIR CARE as much as possible.
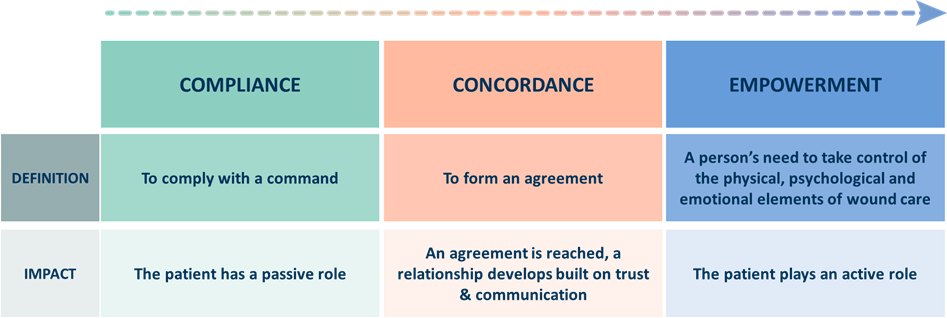
It’s about moving patients from compliance to CONCORDANCE and, where possible, to promote EMPOWERMENT4
How to improve concordance, and therefore the healing outcome ?
The aim is to treat the person, not just the disease.
The quality of dialogue between the healthcare professional & the patient is key to ensuring that effective treatment is implemented.
The dialogue should also involve the patient’s caregivers, who may play a central role in their care.

How to implement inclusive dialogue with a patient presenting with a wound?
1/ Ensure that your patient feels part of the choices made through ACTIVE LISTENING
30% of our communication is verbal and 70% is non-verbal. The goal is, to listen to the person and provide them with empathetic understanding.
There are also five steps that can help to implement active listening, the S.O.L.E.R method4:
Squarely face the person.
Open posture.
Lean towards the person.
Eye contact.
Relax.
But the key is to adapt to the patient AND to their disease.It is important look at the patient and take into consideration:
- Physicial abilities
- Cognitive abilities
- Psychosocial environment
The key question is what is my patient capable of accepting and doing ?
Example of questions to ask for a leg ulcer patient6:
- What is the worst thing/most painful about your leg ulcer?
- Do you have any worries about your treatment plan?
- Explain to me how is it affecting your life.
2/ Always explain the rationale for the decisions that are made and the role they can play, through PATIENT EDUCATION TOOLS
Have a look at our LEGS GO! and SAVEFEETSAVELIVES programs which aim to promote inclusive dialogue
References

